What
The Sentinel Events Registry (SER) tracks reportable events in healthcare facilities. NRS 439.800
1) Have a Patient Safety Officer.
2) Hold Patient Safety meetings.
3) Enroll in the Sentinel Events Registry's reporting platform (REDCap).
4) Complete the facility's 'Contact Form'.
5) Report sentinel events within the NRS timelines, including reporting part 2 the 'RCA' or Root Cause Analysis.
6) File the Annual Summary Report between January 1 and March 1 of each year, covering the previous calendar years patient safety activities.
Optional: Attend the June State of Nevada's Board of Health meeting where the compiled Annual Report is presented. State of Nevada Board of Health
"In plain terms a sentinel event is anything that should never happen in a healthcare setting."
Nevada Revised Statues 439.830 refers to the National Quality Foundation's NQF Serious Reportable Events for a living document that defines the events that are reportable.
"In plain terms a sentinel event is anything that should never happen in a healthcare setting."
Nevada Revised Statues 439.830 refers to the National Quality Foundation's NQF Serious Reportable Events for a living document that defines the events that are reportable.
|
SER Code |
NQF Reference |
Event Description |
|
100 |
1A |
Surgery (invasive procedure) on wrong site (body part) |
|
110 |
1B |
Surgery (invasive procedure) on wrong patient |
|
120 |
1C |
Procedure complication(s) |
|
121 |
1C |
Wrong surgery (invasive procedure) performed |
|
130 |
1D |
Unintended retained foreign object |
|
140 |
1E |
Intra- or post-operative death |
|
141 |
1E |
Intra- or post-operative permanent harm |
|
200 |
2A |
Use of contaminated drug(s) |
|
201 |
2A |
Use of contaminated device(s) |
|
202 |
2A |
Use of contaminated biologic(s) |
|
210 |
2B |
Device failure |
|
211 |
2B |
Device use other than intended |
|
220 |
2C |
Air embolism |
|
300 |
3A |
Discharge or release of patient/resident unable to make decisions |
|
301 |
3A |
Discharge to other than authorized person - adult (18+) |
|
302 |
3A |
Discharge to other than authorized person - child (2-17) |
|
303 |
3A |
Discharge to other than authorized person - infant (<2) |
|
310 |
3B |
Elopement (disappearance) |
|
320 |
3C |
Suicide |
|
321 |
3C |
Suicide - attempted |
|
322 |
3C |
Self harm |
|
323 |
3C |
Self harm - attempted |
|
400 |
4A |
Medication error (wrong drug) |
|
401 |
4A |
Medication error (wrong dose) |
|
402 |
4A |
Medication error (wrong patient) |
|
403 |
4A |
Medication error (wrong time) |
|
404 |
4A |
Medication error (wrong rate) |
|
405 |
4A |
Medication error (wrong preparation) |
|
406 |
4A |
Medication error (wrong route of administration) |
|
410 |
4B |
Unsafe administration of blood product(s) (transfusion, draw, etc.) |
|
411 |
4B |
Error in administration of blood product(s) (transfusion, draw, etc.) |
|
420 |
4C |
Maternal low risk pregnancy labor |
|
421 |
4C |
Maternal low risk pregnancy delivery |
|
422 |
4C |
Maternal low risk pregnancy intrapartum |
|
430 |
4D |
Neonate low risk pregnancy labor |
|
431 |
4D |
Neonate low risk pregnancy delivery |
|
432 |
4D |
Neonate low risk pregnancy intrapartum |
|
440 |
4E |
Fall |
|
450 |
4F |
Pressure ulcer (stage 3 or 4 or unstageable) |
|
451 |
4F |
Pressure ulcer (stage 3 or 4 or unstageable) with HAI |
|
452 |
4F |
Pressure ulcer (stage 1 or 2) |
|
460 |
4G |
Wrong egg |
|
461 |
4G |
Wrong sperm |
|
470 |
4H |
Specimen Loss (irretrievable and/or irreplaceable) |
|
471 |
4H |
Specimen ID Error |
|
480 |
4I |
Failure to communicate laboratory test result |
|
481 |
4I |
Failure to communicate pathology test result |
|
482 |
4I |
Failure to communicate radiology test result |
|
483 |
4I |
Failure to communicate (other) (includes external communications) |
|
500 |
5A |
Electric shock (faulty equipment-machinery-wiring) |
|
501 |
5A |
Electric shock (Damaged receptacles or connectors or...) |
|
502 |
5A |
Electric shock (Unsafe work practices.) |
|
503 |
5A |
Electric shock (Other) |
|
510 |
5B |
Wrong gas |
|
511 |
5B |
Contaminated gas |
|
512 |
5B |
No gas from system designated for gas to be delivered |
|
520 |
5C |
Burn |
|
530 |
5D |
Use of Physical Restraint(s) |
|
531 |
5D |
Bedrail associated injury |
|
600 |
6A |
Introduction of metallic object into MRI area (staff Injury) |
|
601 |
6A |
Introduction of metallic object into MRI area (patient/resident injury) |
|
700 |
7A |
Impersonation of healthcare professional - physician |
|
701 |
7A |
Impersonation of health-care professional - nurse |
|
702 |
7A |
Impersonation of health-care professional - pharmacist |
|
703 |
7A |
Impersonation of healthcare provider (all others) |
|
710 |
7B |
Abduction - adult |
|
711 |
7B |
Abduction - adult - attempted |
|
712 |
7B |
Abduction - child |
|
713 |
7B |
Abduction - child - attempted |
|
714 |
7B |
Abduction - infant |
|
715 |
7B |
Abduction - infant - attempted |
|
720 |
7C |
Rape |
|
721 |
7C |
Rape - attempted |
|
722 |
7C |
Sexual assault |
|
723 |
7C |
Sexual assault - attempted |
|
724 |
7C |
Sexual abuse |
|
725 |
7C |
Sexual abuse - attempted |
|
730 |
7D |
Physical Assault |
|
730 |
7D |
Physical Assault |
|
731 |
7D |
Physical Assault - Attempted |
|
732 |
7D |
Homicide |
|
733 |
7D |
Homicide - attempted |
|
800 |
8 |
Death - Other than Natural Causes (SB457) |
|
999 |
Determined Not a Sentinel Event (Requires Chief Medical Officer Finding) |
REDCaps is the name of the web based reporting platform for the Sentinel Events Registry. (The SER has used the REDCaps platform since October of 2016.) NO PAPER FORMS.
REDCaps is the technology currently used to enter SER data. This technology is provided free of charge from Vanderbilt university, is considered HIPPA compliant and is also used by the CDC and over 2000 other healthcare related entities worldwide
The interface can be overwhelming at first, as there are many options and the system is meant to provide the ability to conduct surveys, and perform clinical trial data input, in addition to how the State of Nevada’s Sentinel Events Registry has adopted it.
Legislation in 2019 expanded the type of healthcare facilities that must participate in the Sentinel Events Registry. (from 'medical' only, to all 'healthcare' type facilities)
NRS 439.803 “Health facility” defined. “Health facility” means:
1. Any facility licensed by the Division pursuant to chapter 449 of NRS; and
2. A home operated by a provider of community-based living arrangement services, as defined in NRS 449.0026.
(Added to NRS by 2019, 1666)
NRS 439.805 “Medical facility” defined. “Medical facility” means:
1. A hospital, as that term is defined in NRS 449.012 and 449.0151;
2. A freestanding birthing center, as that term is defined in NRS 449.0065;
3. A surgical center for ambulatory patients, as that term is defined in NRS 449.0151 and 449.019; and
4. An independent center for emergency medical care, as that term is defined in NRS 449.013 and 449.0151.
(Added to NRS by 2002 Special Session, 13; A 2021, 3428)
NRS 630.0135 “Medical facility” defined. “Medical facility” has the meaning ascribed to it in NRS 449.0151.
NRS 449.0151 “Medical facility” defined. “Medical facility” includes:
1. A surgical center for ambulatory patients;
2. A freestanding birthing center;
3. An independent center for emergency medical care;
4. An agency to provide nursing in the home;
5. A facility for intermediate care;
6. A facility for skilled nursing;
7. A facility for hospice care;
8. A hospital;
9. A psychiatric hospital;
10. A facility for the treatment of irreversible renal disease;
11. A rural clinic;
12. A nursing pool;
13. A facility for modified medical detoxification;
14. A facility for refractive surgery;
15. A mobile unit; and
16. A community triage center.
(Added to NRS by 1973, 1279; A 1975, 366; 1979, 161, 887, 1113; 1983, 1657; 1985, 1736; 1989, 304, 1035, 1037; 1999, 248, 970; 2001, 1341; 2005, 532, 2693; 2021, 3437)
Table of facility types expected to enroll and participate, and levels of enrollment and participation from 2022.
|
Facility Type Description |
Count of Facility Type |
SER Enrolled |
SER Enrolled Percent |
SER Participant |
SER Participant Percent |
|
Adult Day Care Facility |
30 |
4 |
13.0% |
0 |
0.0% |
|
Alcohol or Drug Treatment Facility |
22 |
8 |
36.0% |
1 |
5.0% |
|
Ambulatory Surgical Center |
88 |
77 |
88.0% |
29 |
33.0% |
|
Community Triage Center |
2 |
1 |
50.0% |
0 |
0.0% |
|
Domestic Violence Treatment Programs |
27 |
0 |
0.0% |
0 |
0.0% |
|
Freestanding Birthing Center |
1 |
0 |
0.0% |
0 |
0.0% |
|
Half-Way House for Recovering |
9 |
0 |
0.0% |
0 |
0.0% |
|
Hospice Care Facility |
187 |
32 |
17.1% |
20 |
10.7% |
|
Hospital |
51 |
50 |
98.0% |
39 |
76.0% |
|
Independent Emergency Medical Care |
1 |
1 |
100.0% |
0 |
0.0% |
|
Individual Residential Care Homes |
121 |
13 |
11.0% |
2 |
2.0% |
|
Intermediate Care Facility |
9 |
1 |
11.1% |
1 |
11.1% |
|
Medical Detoxification Facility |
10 |
4 |
40.0% |
0 |
0.0% |
|
Medication Unit |
1 |
0 |
0.0% |
0 |
0.0% |
|
Narcotics Treatment Facility |
15 |
1 |
7.0% |
1 |
7.0% |
|
Nursing Care in the Home Agency |
225 |
51 |
22.7% |
23 |
10.2% |
|
Nursing Pool |
57 |
14 |
25.0% |
11 |
19.0% |
|
Outpatient Facility |
51 |
18 |
35.0% |
10 |
20.0% |
|
Personal Care Agency |
294 |
58 |
19.7% |
14 |
4.8% |
|
Psychiatric Residential Treatment Facility |
15 |
0 |
0.0% |
0 |
0.0% |
|
Recovery Center Facility |
3 |
2 |
67.0% |
0 |
0.0% |
|
Renal Disease Treatment Facility |
55 |
33 |
60.0% |
1 |
2.0% |
|
Residential Group Facility |
400 |
111 |
28.0% |
26 |
6.0% |
|
Rural Clinic |
20 |
2 |
10.0% |
0 |
0.0% |
|
Rural Hospital |
15 |
15 |
100.0% |
12 |
80.0% |
|
Skilled Nursing Facility |
67 |
26 |
38.8% |
9 |
13.4% |
|
Total |
1,776 |
522 |
29.4% |
199 |
11.2% |
In June of 2022 the Deputy Attorney General provided the following briefing regarding exemptions.
Regarding: Develop NRS Exemption(s) to address certain facility types, concerning 1) possible double reporting and 2) workers in client’s home
NRS states the following Bureau of Health Care Quality and Compliance (HCQC) HCQC licensed facility types must participate in the Sentinel Events Registry.
NRS 439.835 requires that medical facilities (and healthcare facilities added in 2019) report sentinel events to DPBH (Sentinel Events Registry).
NRS 449.803 defines “Health facility”, while NRS 439.805, defines “Medical facility” as HCQC licensed entity types required to report sentinel events.
Summary of Deputy Attorney General’s determination:
If the entity is permitted pursuant to Chapter 449 of NRS, so the entity would meet the
definition of a health facility in NRS 439.803 which is the appropriate definition to use in
regards to sentinel event reporting.
If the entity can be searched as a ‘healthcare facility’ at HCQC’s website,
https://nvdpbh.aithent.com/login.aspx then they are expected to participate in the Sentinel
Events Registry.
Explanation of why an exemption was inquired about.
Nursing Pool (NRS 449.0153)
In particular, the license type of ‘Nursing Pool’ by it’s business model, deploys professionally qualified staff to settings owned and operated by other license types that are included in the list of expected reporting facility types. This leads to unintended consequences that could result in
1) duplicate reporting,
2) excessive delay in reporting, and
3) Inability to have appropriate information for purposes of reporting. (attachments)
Personal Care Agency, and other
Other license types that provide services in the clients home or services have asked for special reduced burden in as much as the location of service is a domestic setting and not a ‘Health facility’ per say.
Personal Care Agency’s state that their service array consists of only light housekeeping, bathing,
dressing, and grooming, while some simply check on clients at regular schedules. Substance Abuse Treatment programs have put forth the argument that they do no health or medical service.
1 day (24 hours) - (Staff awareness to notify Patient Safety Officer) A person who is employed by a healthcare facility shall after becoming aware of a sentinel event that occurred at the healthcare facility, notify the patient safety officer of the facility of the sentinel event.
7 days - (Provide notification to patient/resident) Not later than 7 days after discovering or becoming aware of a sentinel event that occurred at the healthcare facility, provide notice of that fact to each patient who was involved in that sentinel event. (NRS 439.855)
13 or 14 days - (Report event to the SER by creating and completing Event Report Part 1) Report to the division, depending on whether the patient safety officer personally discovers (13 days) or becomes aware of the sentinel event or the other healthcare employee at the healthcare facility discovers or becomes aware of the sentinel event and must inform the patient safety officer (14 days). Reports are initiated by utilizing the Part 1 form. (NRS 439.835)
45 Days -(Report event Root Cause Analysis to the SER by creating and completing Event Report Part 2) Within 45 days of receiving notification or becoming aware of the occurrence of a sentinel event, the facility is required to submit the Part 2 form, which includes the facility’s quality improvement committee describing key elements of the events, the circumstances surrounding their occurrence, the corrective actions that have been taken or proposed to prevent a recurrence, and methods for communicating the event to the patient’s family members or significant other(s). (NAC 439.915)
Calendar Year - (Between January 1 and March 1 complete the Patient Safety Activities Annual Summary Report filing) The Annual Summary Report is due by the close of business on March 1 of each year, for the proceeding years’ patient safety activities at your facility. (NRS 439.843)
If you represent more than one facility, that should be noted on the 'New User Agreement'. The form will ask how many facilities you will represent, then you will add the names, HCQC license number, facility type, etcetera. Then you will use the 'Data Access Group' switcher to select which facility for reporting each time you enter a reporting project. The 'DAG' switcher uses the facilities State of Nevada HCQC license number to indicate the facility.
If a single account needs to represent more than one facility, the New SER Account form can accommodate collecting the needed information. You will need to complete the ‘User Agreement’ survey form linked below.
For a new REDCap account for the Sentinel Events Registry (SER) program, or any other program that uses the REDCap platform please complete this survey form.
Your primary contact email MUST be unique to you.
If required fields are left blank, the process will be delayed while the needed information is asked for through an email. Please do not put commas in fields. If a field does not apply to you enter ‘NA’.
https://redcap.link/REDCAP_USER
Once completed, send an email to ser@health.nv.gov, and or the SER administrator email, that the new account survey has been completed. The intent is that within 10 business days of your completing the survey, your new account will be created.
Each account’s email address MUST be unique.
Once your account is created, you will receive an email to set your account password.
REDCap uses two factor email authentication. When logging in you will see a pop up window (may need to allow pop ups), simply click on the gray radio button. Then check your account’s email. Copy and paste the 6 digit code into the pop up dialog box, and press enter.
If the facility accepted patients at any time during the reporting period, then the facility Contact Form, and the Sentinel Event Annual Summary report must be completed.
When a change occurs in name, ownership, or license number, inform the SER, so that a new Contact Form can be completed.
Natural Deaths versus Non-Natural Deaths. A new reporting requirement, in addition to serious reportable events found in the NQF definition. To help understand the meaning of the term the following is provided:
Natural is defined as death caused solely by disease or natural process. If natural death is hastened by injury (such as a fall or drowning in a bathtub), the manner of death is not considered natural. (Non-Natural Death and now requires reporting to the Sentinel Events Registry)
In 2019, SB457 was passed during the 80th session of Nevada’s Legislature. This bill modified and expanded the State of Nevada Sentinel Events Registry (NRS 439.800) and other healthcare facility reporting requirements.
In addition to the expanded list of healthcare facilities now required to report sentinel events, the reporting of any death in a healthcare facility is required (not related to NQF), with the exception of a “death due to natural causes” as understood in a general meaning and for which it has been established that the cause of death is not due to any contributing factors by the healthcare facility.
Though no facility has been fined to date, low participation rates may cause a change in policy.
NRS 439.885 Violation by health facility: Administrative sanction prohibited when voluntarily reported; administrative sanction imposed when not voluntarily reported; appeal of imposition of sanction; accounting and expenditure of money.
1. If a health facility:
(a) Commits a violation of any provision of NRS 439.800 to 439.890, inclusive, or for any violation for which an administrative sanction pursuant to NRS 449.163 would otherwise be applicable; and
(b) Of its own volition, reports the violation to the Administrator,
Ê such a violation must not be used as the basis for imposing an administrative sanction pursuant to NRS 449.163.
2. If a health facility commits a violation of any provision of NRS 439.800 to 439.890, inclusive, and does not, of its own volition, report the violation to the Administrator, the Division may, in accordance with the provisions of subsection 3, impose an administrative sanction:
(a) For failure to report a sentinel event, in an amount not to exceed $100 per day for each day after the date on which the sentinel event was required to be reported pursuant to NRS 439.835;
(b) For failure to adopt and implement a patient safety plan pursuant to NRS 439.865, in an amount not to exceed $1,000 for each month in which a patient safety plan was not in effect; and
(c) For failure to establish a patient safety committee or failure of such a committee to meet pursuant to the requirements of NRS 439.875, in an amount not to exceed $2,000 for each violation of that section.
3. Before the Division imposes an administrative sanction pursuant to subsection 2, the Division shall provide the health facility with reasonable notice. The notice must contain the legal authority, jurisdiction and reasons for the action to be taken. If a health facility wants to contest the action, the facility may file an appeal pursuant to the regulations of the State Board of Health adopted pursuant to NRS 449.165 and 449.170. Upon receiving notice of an appeal, the Division shall hold a hearing in accordance with those regulations.
4. An administrative sanction collected pursuant to this section must be accounted for separately and used by the Division to provide training and education to employees of the Division, employees of health facilities and members of the general public regarding issues relating to the provision of quality and safe health care.
(Added to NRS by 2002 Special Session, 16; A 2005, 600; 2009, 554; 2011, 680; 2013, 3042; 2019, 1671)
NRS 439.875 Patient safety committee: Establishment; composition; meetings; duties; proceedings and records are privileged.
3. The Administrator shall adopt regulations prescribing the composition and frequency of meetings of patient safety committees at medical facilities having fewer than 25 employees and contractors.
In practice this means the expectation for 25 or fewer employees and contractors to hold patient safety meetings at least quarterly, while those with more than 25 employees and contractors are expected to hold patient safety meetings at least once a month.
In all instances, the expectation is that attendance is required of all appropriate staff.
When entering values for this in the Annual Summary report and on the Contact Form, please enter what is occurring at your facility.
How
For a new REDCap account for the Sentinel Events Registry (SER) program, or any other program that uses the REDCap platform please complete this survey form in the link below.
If changes need to be made to an existing account, use the same link.
In both cases, please send an email to the SER Administrator, and to the SER email account informing the need for a new account and/or change to an existing account.
If a single account needs to represent more than one facility, the New SER Account form can accommodate collecting the needed information.
Your primary contact email MUST be unique to you.
If required fields are left blank, the process will be delayed while the needed information is asked for through an email. Please do not put commas in fields. If a field does not apply to you enter ‘NA’.
https://redcap.link/REDCAP_USER
Once on the web browser, scroll down to see the area for input of information.
A new account will be created within 10 business days ( or sooner if possible, hopefully not later). Each role at your facility, Patient Safety Officer(required), Designated Reporter1(optional), and Designated Reporter2(optional) accounts need to complete the survey.
Pre-requisites:
You already have a patient safety role at your facility, such as Patient Safety Officer, or one of the two Designated Reporters.
You already have a REDCap reporting platform account.
Start:
Login to the REDCap platform. State of Nevada REDCap https://dpbhrdc.nv.gov/redcap/ 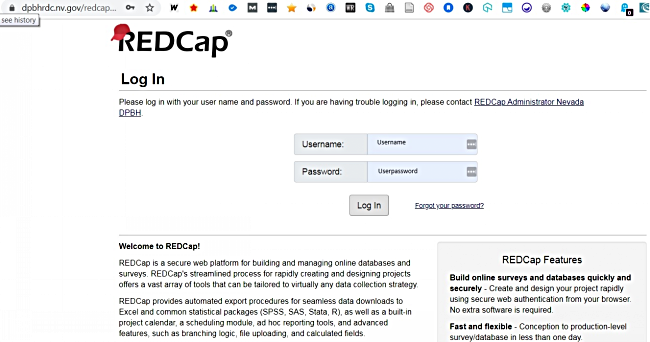
Enter your username and password. (must login every 6 months to avoid account suspension)
Click radio button to initiate two factor 6 digit code..2.png)
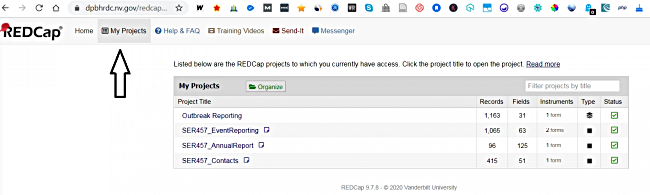
Navigate to the 'My Projects' link near the upper left of the page. Select one of the following based on the purpose.
Pre-requisites:
You already have a patient safety role at your facility, such as Patient Safety Officer, or one of the two Designated Reporters.
You already have a REDCap reporting platform account.
Login to the REDCap platform. State of Nevada REDCap
Enter your username and password. (must login every 6 months to avoid account suspension)
Click radio button to initiate two factor 6 digit code.
Click on 'My Project'.
Start:
Navigate to the 'My Projects' link near the upper left of the page. Select one of the projects that you see based on the reporting purpose.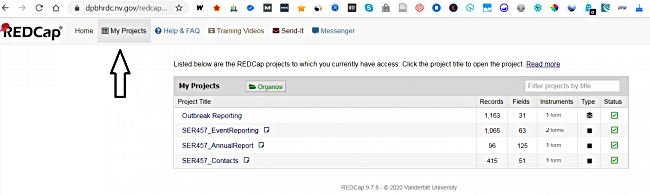
Pre-requisites:
You already have a patient safety role at your facility, such as Patient Safety Officer, or one of the two Designated Reporters.
You already have a REDCap reporting platform account.
You are inside the SER_EventReporting project.
Start:
On the left hand panel under the heading 'Data Collection' to enter a new event select 'Add / Edit Records'.
On the left hand panel under the heading 'Data Collection' to view all existing events select 'Record Status Dashboard'.
.1.jpg)
Pre-requisites:
You already have a patient safety role at your facility, such as Patient Safety Officer, or one of the two Designated Reporters.
You already have a REDCap reporting platform account.
You are inside the SER_EventReporting project.
You have selected 'Add / Edit Records'
Start:
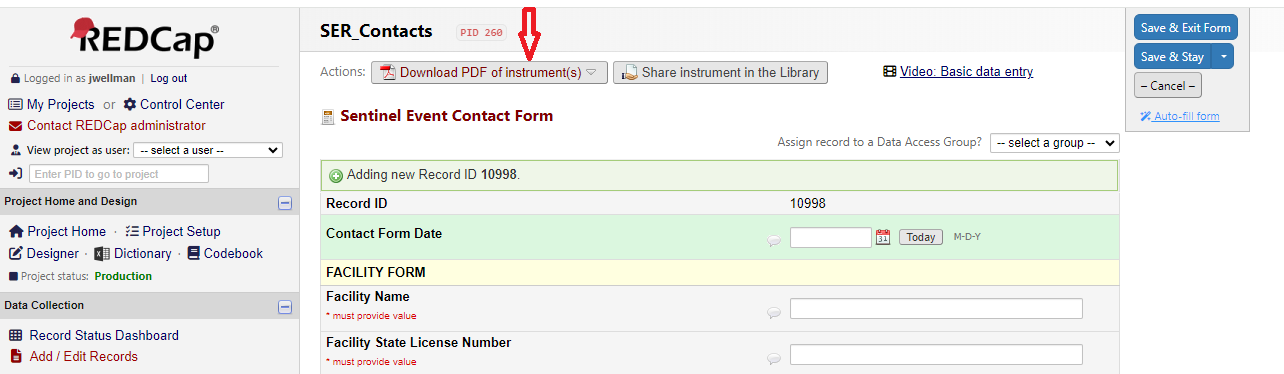
Click the '+Add new record' green button.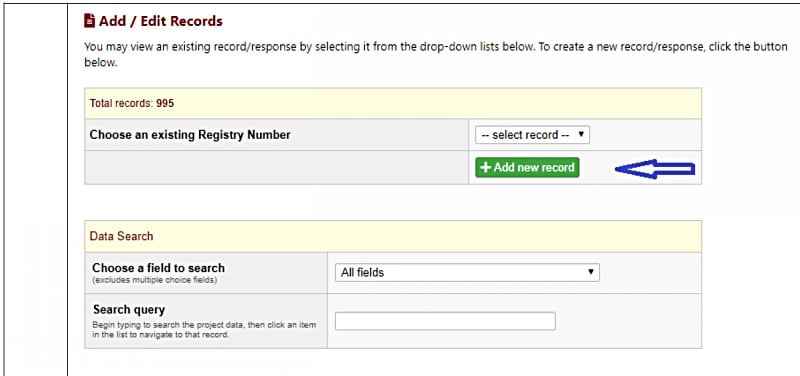
Next, select the gray radio button to access the forms.
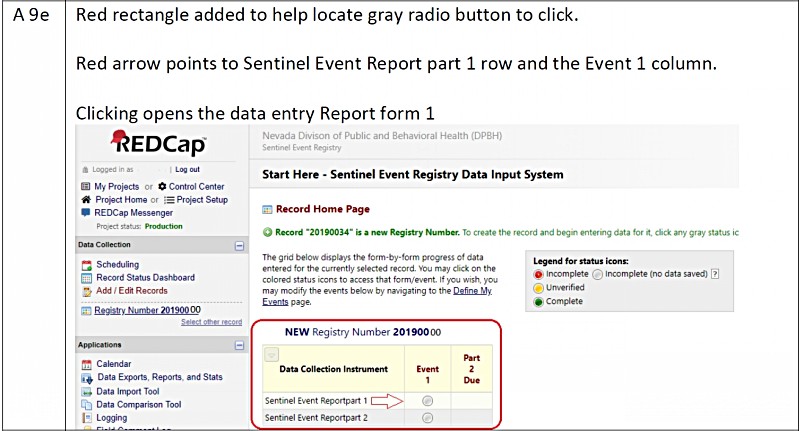
Complete all fields that apply. Fields with an '* Must provide value' in red will not allow you to save until a value has been entered.
When complete, change status to 'Unverified', save and exit.
When the SER staff review, a permanent record ID is assigned, and the status changed to 'Complete'.
Be sure that the patient's date of birth is correct, and not accidentally entered as 'today'.
You will only hear from the SER in regard to the filing if the information input is not complete.
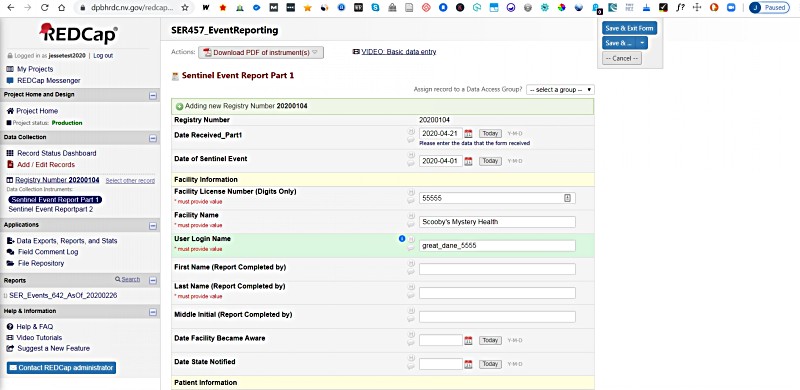 Select 'Unverified', then 'Save & Exit Form'.
Select 'Unverified', then 'Save & Exit Form'.
Download a pdf version of the Sentinel Events Registry ReportPart1 Notify the State.
Pre-requisites:
You already have a patient safety role at your facility, such as Patient Safety Officer, or one of the two Designated Reporters.
You already have a REDCap reporting platform account.
You are inside the SER_EventReporting project.
You have selected 'Add / Edit Records'
You have completed ReportPart1, notifying the Sentinel Events Registry of a sentinel event.
You have conducted a root cause analysis, including interviewing both staff and non staff, reviewed the event, and provided administration of the findings.
Start:
Select the gray radio button to access the forms.
Complete all fields that apply. Fields with a '*Must provide value' in red must be completed or the record will not be saved.
When complete, change status to 'Unverified', save and exit.
When the SER staff review, a permanent record ID is assigned, and the status changed to 'Complete'.
Be sure that the patient's date of birth is correct, and not accidentally entered as 'today'.
You will only hear from the SER in regard to the filing if the information input is not complete.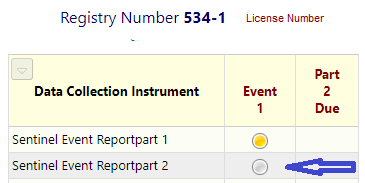
Complete all fields as applicable. You will be asked to provide general and detailed factors, number of staff and non staff interviewed, any lessons learned, any change in policy or procedures, and the date that administration was provided the findings.
When complete, select 'Unverified', then 'Save & Exit Form'.
Download a pdf version of the Sentinel Events Registry ReportPart2 Root Cause Analysis findings.
Pre-requisites:
You already have a patient safety role at your facility, such as Patient Safety Officer, or one of the two Designated Reporters.
You already have a REDCap reporting platform account.
You are inside the SER_EventReporting project.
You have selected 'Add / Edit Records'
You have entered all values in the data entry form. Checked dates so no patient/resident born today, unless a newborn. No event date after staff learned of event. All fields with a red note are required.
Start:
Now you are ready to save the record.
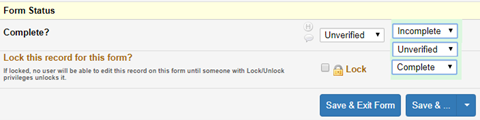
Choose 'Unverified' from the drop-down list. When a SER Staff member reviews and finds no data issues, the record is assigned a id, and the status is changed to 'Complete', and locked. Only records with data issues will be contacted by the SER.
Pre-requisites:
You already have a patient safety role at your facility, such as Patient Safety Officer, or one of the two Designated Reporters.
You already have a REDCap reporting platform account.
You have logged in to REDCap (see questions above)
You have selected 'My Projects', then select the project 'SER_AnnualReport'.
You are inside the SER_AnnualReport project.
You have selected 'Add / Edit Records' found on the left hand panel under the 'Data Collection' header.
Start:
Click on the green button '+Add new record'.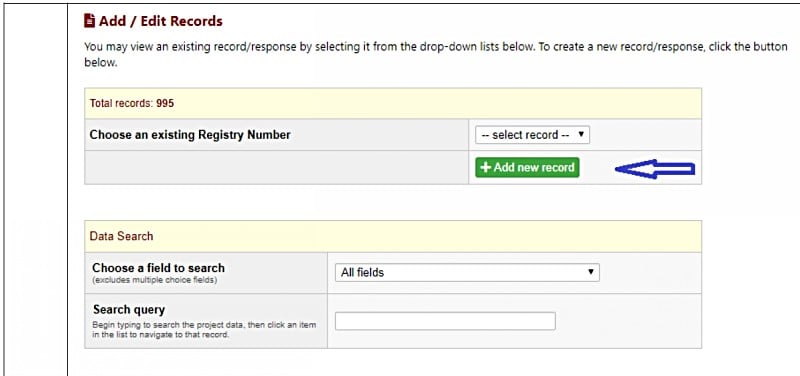 Start at the top completing each question. If there was no sentinel events in the reporting calendar year, enter a value of 0 (zero). (hint: use the tab key to quickly move between textboxes)
Start at the top completing each question. If there was no sentinel events in the reporting calendar year, enter a value of 0 (zero). (hint: use the tab key to quickly move between textboxes)
Download a pdf file of the form (dec2023 edition)
Send an email to the Administrator, and the SER email account informing of the staff changes.
You will be contacted asking for the accounts to be made inactive, any new staff that need an account (must complete the New User Agreement), and a link to your facility's Contact Form asking that all values be 'made current'. Each role is exclusive to one person. (a single person should not be listed twice on the Contact Form)
This is an example of the Contact Form. SER Contact Form Dec23
Near the upper left of each form is a button option to print the form to a pdf file.
In all cases, when filing an individual sentinel event report part 1, report part 2, the Annual Summary report, and an update/change to a Contact Form, save the record with a status of 'Unverified'.
In all cases, when filing an individual sentinel event report part 1, report part 2, the Annual Summary report, and an update/change to a Contact Form, save the record with a status of 'Unverified'.
The status will remain 'Unverified' until SER staff review the record. If everything is ok, the status will be changed to 'Complete', and the record locked.
YOU WILL ONLY BE CONTACTED REGARDING A SUBMISSION IF THERE IS A NEED FOR CLARRIFICATION.
The reporting person will only be contacted if the record needs additional information or correction of information. (Most common reasons are a dates that look out of place, or critical required fields not completed.)
Be sure to verify facility-became-aware, notification of the Patient Safety Officer, and notified-the-patient dates.
Do not under any circumstance enter a value of 'not a sentinel event' in the event drop down list.
If you made a mistake, contact the SER Administrator and the SER email asking for help to fix any issues.
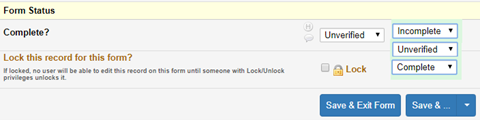
When submitted, the status will be 'Unverified' orange.
When reviewed by staff and accepted, the status will be 'Complete' green.
On the lower left, inside the white background panel titled 'New Applicants Apply Here', and then locate "LICENSE VERIFICATION, FACILITY LOCATOR & INSPECTION REPORTS (personnel/health facility/laboratory/kitchen pool & spa) Click Here"
The URL will look like this. https://nvdpbh.aithent.com/Protected/LIC/LicenseeSearch.aspx?Program=HFF&PubliSearch=Y&returnURL=~/Login.aspx?TI=0#noback
Business Unit > 'Health Facilities'.
Facility Name > here is where you enter your facility's name.
Select the 'Search' button.
In the results provided, look to the column titled 'Credential Number'. The digits on the left are needed for the SER program.
For word it is ‘run the accessibility checker’.
Word instructions to check for ADA compliance
There are other sources to check. Also be sure to redact staff names as the Patient Safety Plan will become publicly discoverable.
